Managing Monkeypox: Take 3 Steps Now to Protect Patients and Staff
After three long years of managing COVID-19, the world is facing another public health crisis: monkeypox.
According to the World Health Organization, “Monkeypox is a viral zoonotic disease that occurs primarily in tropical rainforest areas of central and West Africa, and is occasionally exported to other regions.” Humans can get monkeypox through close contact with an infected person or animal, or with contaminated material. In turn, they can spread it to other humans through close contact with lesions, respiratory droplets, body fluids, and contaminated items such as sheets and pillowcases. Monkeypox usually causes a fever, a painful rash that turns into blisters, and swollen lymph nodes.
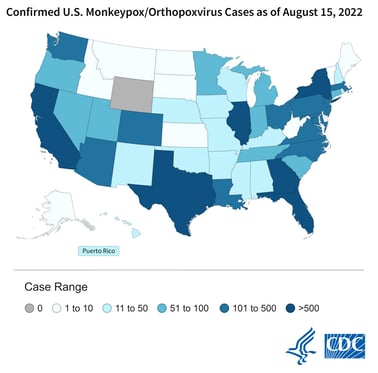
In May of this year, cases of monkeypox became more wide-spread, especially in regions not typically known to experience the disease. Monkeypox was identified in 89 counties, 82 of which historically have not had monkeypox outbreaks. In the United States, cases have been identified in all but one state, with 11,890 cases total. More than 500 cases each have been identified in Florida, California, Georgia, and Illinois. On August 4, 2022, the U.S. Department of Health and Human Services (HHS) declared monkeypox a public health emergency.
ECRI recommends taking these 3 steps:
1) Implement Screening
Screen patients as soon as they enter your healthcare facility, during registration. Especially in emergency departments, urgent care centers, and ambulatory clinics, screening is critical to containing the virus, effectively caring for patients, and protecting staff. Implement a checklist to be used when patients enter your facility, and determine if they meet any of the Epidemiologic Criteria as defined by the Centers for Disease Control and Prevention (CDC), or present with a new characteristic rash consistent with monkeypox. If a patient is positive, the healthcare facility must implement its policy to manage suspected or confirmed cases (i.e. placing in single room, transporting with mask, appropriate personal protective equipment).
2) Require Personal Protective Equipment (PPE)
Although many healthcare workers are facing PPE fatigue, it is imperative that organizations continue to enforce proper use of PPE as listed by the CDC (e.g., gowns, gloves, NIOSH-approved particulate respirators equipped with N95 filters or higher). Organizations must also ensure supply and ease of access to appropriate PPE.
3) Education
Lastly, organizations must educate all healthcare workers, clinical and non-clinical, about the transmission of monkeypox. For both groups, the correct use of PPE is critical. For non-clinical workers, it is important to provide information about how to safely handle potentially contaminated linens and laundry appropriately.
Use this ECRI policy development guide that details what to include when creating a monkeypox policy.
For additional assistance contact us today at clientservices@ecri.org.
