Evidence-based Strategies for Preventing CAUTIs from Indwelling Catheters
According to the Centers for Disease Control and Prevention (CDC), urinary tract infections (UTIs) are the most common healthcare-associated infection, and approximately 75% of UTIs acquired in the hospital are catheter-associated urinary tract infections (CAUTIs).
Urinary catheters interfere with the natural host defense of clearing the bladder and urethral mucosa of microbes through voiding. The catheter also acts as a direct entry portal into the bladder for nearby microorganisms. Pathogens can access the urinary tract either from outside the catheter or from a contaminated collection bag or catheter-drainage tube connection. Many bacterial species colonize indwelling catheters as a thin, slimy film that adheres to a surface. In this form, bacteria are resistant to antibiotics and host defenses.
Risk factors for CAUTI include:
- Prolonged catheterization
- Female gender
- Older age
- Having diabetes mellitus
- Bacterial colonization of the drainage bag
- Errors in catheter care, such as not adhering to sterile technique or not maintaining a closed drainage system
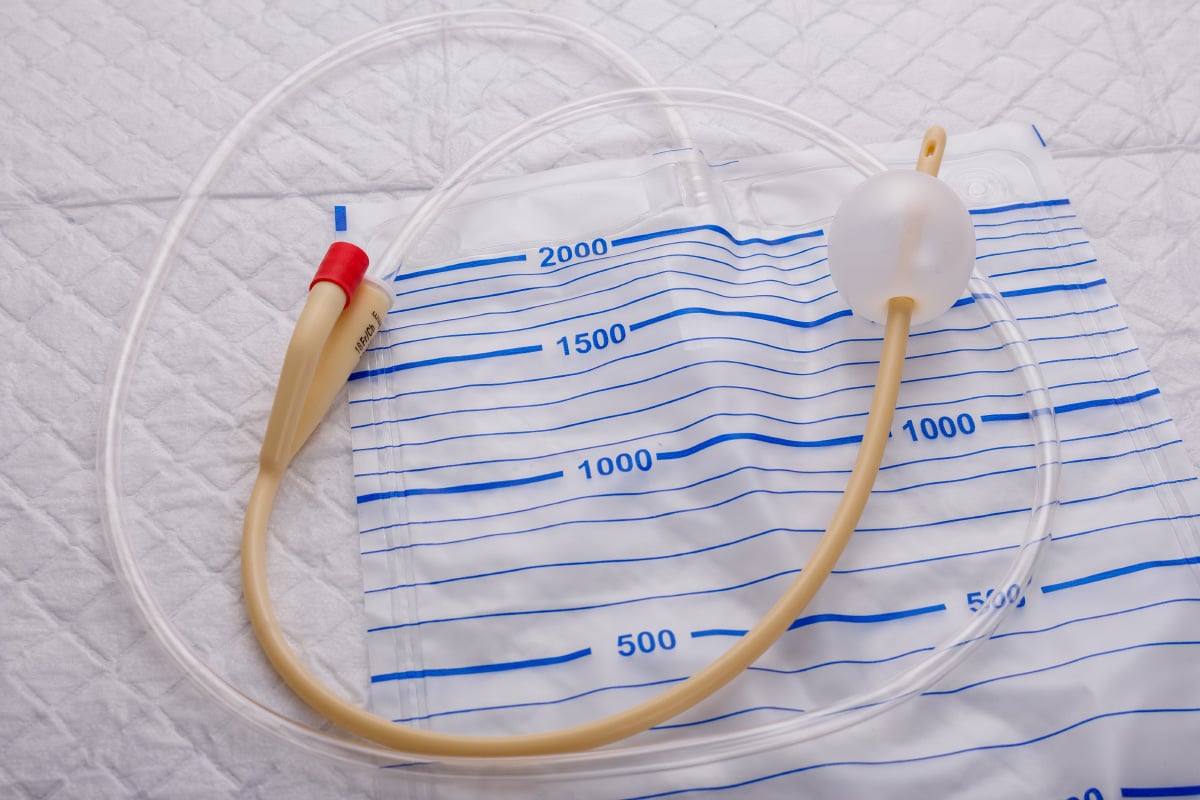
Indwelling Urinary Catheters
Indwelling catheters are inserted to treat chronic medical conditions that impede urine flow from the bladder as it exits the body. Urinary catheter uses include:
- Treatment of urinary retention
- Monitoring of urinary output volume
- Medical instillation
- Treatment of urinary tract obstruction
- Treatment of neurogenic bladder dysfunction
- Postoperative management of surgical patients
Indwelling urinary catheters may be inserted directly into the urethra (urethral catheter) or through a tube inserted through small holes made in the skin and underlying bladder wall (suprapubic catheter). According to CDC, “15-25% of hospitalized patients receive urinary catheters during their hospital stay."
CAUTI Prevention Strategies
According to ECRI’s recent Clinical Evidence Assessment, Evidence-based Strategies for Preventing Catheter-associated Urinary Tract Infections from Indwelling Catheters, a wide range of evidence-based interventions are available for preventing CAUTIs. Specific approaches depend on the patient's medical condition. Interventions supported by evidence from systematic reviews include:
- Hydrophilic-coated catheters or other types of coated catheters for long-term catheterization
- Bladder instillation
- Removal of short-term indwelling catheters
- Removal of catheters early after surgery
- Urethral cleaning
Recent clinical practice guidelines emphasize several UTI prevention strategies, including:
- Appropriate use of indwelling catheters
- Aseptic technique for insertion
- Maintenance of a closed system
- Maintenance of an unobstructed urine flow
- Timely removal
- Surveillance
- Education
A guideline from the European Association of Urology states: “Indwelling catheters should be placed only when they are clinically indicated; for example, for management of urinary retention or where strict monitoring of fluid balance is required.”
A University of Michigan Health System guideline recommends: “Avoid catheterization whenever possible. When it is needed, limit the duration of catheterization, and use clean intermittent catheterization instead of an indwelling catheter."
A guideline from the Scottish Intercollegiate Guidelines Network recommends: “Patients with indwelling catheters should have regular review to assess the ongoing need for catheterisation, including consideration of alternatives to catheterisation and trial without catheter."
For patients with neurogenic lower urinary tract dysfunction (NLUTD), a guideline from the American Urological Association recommends:
- “Clinicians should recommend intermittent catheterization rather than indwelling catheters to facilitate bladder emptying in patients with NLUTD.
- For appropriately selected NLUTD patients who require a chronic indwelling catheter, clinicians should recommend suprapubic catheterization over an indwelling urethral catheter.
- In NLUTD patients who perform clean intermittent catheterization with recurrent urinary tract infection, clinicians may offer oral antimicrobial prophylaxis to reduce the rate of urinary tract infections following shared decision-making and discussion regarding increased risk of antibiotic resistance.
- In NLUTD patients who perform clean intermittent catheterization with recurrent urinary tract infection, clinicians may offer bladder instillations to reduce the rate of urinary tract infections.”
Impact
CAUTIs may increase patient morbidity and mortality as well as costs. The U.S. Centers for Medicare & Medicaid Services targets hospitals with higher CAUTI rates for lower reimbursements, which may also exacerbate racial disparities in healthcare delivery.
Learn how ECRI’s Clinical Evidence Assessment service supports clinicians by researching evidence-based strategies for improving patient safety and care quality.
