Drug Diversion and Infection Prevention: When the Needle Hits the Vein
Longtime infection prevention leaders likely remember the story of David Kwiatkowski—a healthcare worker whose drug diversion activities put thousands of patients at risk of hepatitis C infection. Kwiatkowski, who worked as a traveling radiology technician, had a “system” for diverting drugs from his employers. “He would steal vials of painkillers, inject the drugs, and then cover his tracks in various was including methods that lead to his blood tainting vials of medication of which was delivered into patients.”
For years, Kwiatkowski evaded detection as he moved among different hospitals in different states. Even when he was caught and terminated from one facility, liability concerns kept administrators from taking further action. As a result, at least 45 patients contracted hepatitis C. One person died.
Today, hospitals and their patients are safe from Kwiatkowski as he serves a maximum sentence of 39 years. Yet drug diversion remains an issue everywhere—and the Kwiatkowski example illustrates the need for infection prevention teams to pay close attention to this phenomenon.
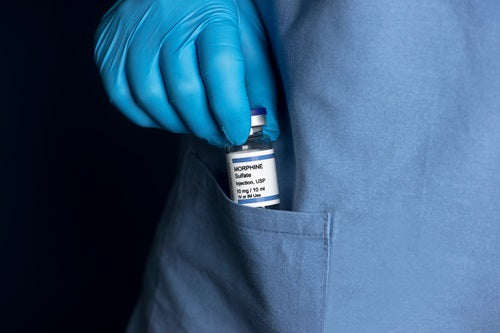
Diversion targets and techniques
Drug diversion in any form increases the risk that a patient will develop an infection. Diversion can even contribute to an outbreak.
Diverters employ a variety of “creative” approaches to gain access to drugs while on the job. As hospitals have invested in safeguards, these workers have found ways to tamper with and defeat them.
For example, nurses have discovered a punctured and drained opioid bag inside an infusion lockbox. Although the box appeared to be secure, the lock could be opened with a paper clip. ECRI lab testing has confirmed similar ways of defeating other locks and secure containers. Even electronic locks with auditing capability and tracking can have limitations.
Diverters can leverage vulnerabilities in other resources, too—including tubing and bags, automated dispensing cabinets, intravenous bag lock boxes that are easily defeated, locks on those boxes that are easily picked, and vials and pre-filled syringes.
No matter how a diverter compromises controls, the result is a chain of events that puts patients and workers at risk. In addition to infection risk, patients may not receive sufficient pain medication or anesthesia, and they could be otherwise harmed by substandard care from an impaired healthcare worker.
Besides putting themselves at risk of overdose or death, diverters could face regulatory penalties, criminal prosecution, and/or malpractice suits due to their drug abuse. For their employers—hospitals and health systems—diversion costs can spiral quickly in the form of investigation costs, compromised patient care, financial penalties and fines, and loss of the diverted medications.
Infection prevention: Break the chain
If you haven’t identified diversion within your organization, you may not be looking hard enough. For infection prevention teams, robust surveillance can help break the chain of infection. Assess facility and organization awareness by studying pharmacy data, clinical data, and quality audits and by engaging with human resources and other staff. Establish a surveillance system to identify and treat newly acquired hepatitis C and other infections, and focus on these five target points for diversion:
- Diverters may remove a purchase order from records or steal DEA 222 forms. Address the risk by working with authorized purchasers and using clear processes for product selection and receipts. In addition to limiting the number of individuals with authorization to purchase, ensure that someone other than the purchaser receives and verifies every delivery.
- Diverters may replace one product with another or remove volume from pre-mixed infusions. Create controls by being intentional about the location of medication storage and practices for verifying inventory and separating products. Ensure that storage offers limited access and is not only secured but also monitored. Perform inventory count verification on a regular basis, using a blinded count where possible. Consider strategies to separate products in storage locations.
- Diverters may forge prescriptions on stolen pads or submit verbal prescriptions not verified by a provider. Thwart them by making sure that prescription pads are secure and locked away—and that only a limited number of authorized individuals have access to them. Also, eliminate the use of verbal orders (if used routinely), and use verbal nursing orders only in urgent/extreme situations when it's not possible to communicate electronically or in writing.
- Diverters may take a medication but still document that it was given as prescribed, or they may divert drugs that should be managed as waste. Define and monitor compliance with PAR levels—ensuring that removal, delivery, and receipt are double-checked and audited. Where possible, use barcode verification, and audit any manual calculations.
- Diverters may take expired drugs and/or remove drug waste from the waste container. Keep a variety of doses on hand to avoid waste, and make sure that medications have tamper-evident packaging. Avoid storing partial packages, too.
Team up to thwart diversion
Reduce the risk of drug diversion—and associated infections—with a proactive, multidisciplinary Controlled Substance Diversion Prevention Program. Infection prevention leaders need to collaborate with other disciplines to prevent, identify, report, and respond to drug diversion.
Your multidisciplinary team can explore numerous tactics for improving detection. These may include physical security measures, such as cameras, as well as electronic methods, such as monitoring prescribing and performing audits and reconciliations. In addition, machine learning diversion monitoring and analytics may help in surfacing anomalies that human eyes might otherwise miss.
Implement a policy requiring real-time reporting of all discrepancies and establish a reporting platform that supports staff who come forward with concerns. Equally important is committing to investigating and responding immediately to any reported suspicions.
Learn more about how ECRI can support you in breaking the chain of infection.
